By Michael Dakkak DO
Dr. Dakkak is a fellowship-trained sports medicine physician practicing at Cleveland Clinic Weston Hospital in Florida. He specializes in non-surgical treatment options for treating orthopedic injuries or chronic pain.
is a fellowship-trained sports medicine physician practicing at Cleveland Clinic Weston Hospital in Florida. He specializes in non-surgical treatment options for treating orthopedic injuries or chronic pain.
Not all hip pain is the same.
Gluteal tendinopathy can be a source of chronic hip pain leading to significant discomfort and affecting a patient’s ability to walk and sleep. Without timely and effective treatment, many patients end up living with pain for much longer than is necessary.
Fortunately, patients can be treated using novel, minimally invasive techniques to relieve their symptoms.
Advancements in ultrasound-guided procedures using innovative medical devices like TenJet allow physicians to treat chronic gluteal tendinopathy, often without the pain and lengthy recovery required by traditional forms of surgery.
Here’s a closer look at gluteal tendinopathy and why a minimally invasive treatment using TenJet may be exactly what’s needed to give patients relief from chronic hip pain and get them back to their active lifestyles.
What is gluteal tendinopathy?
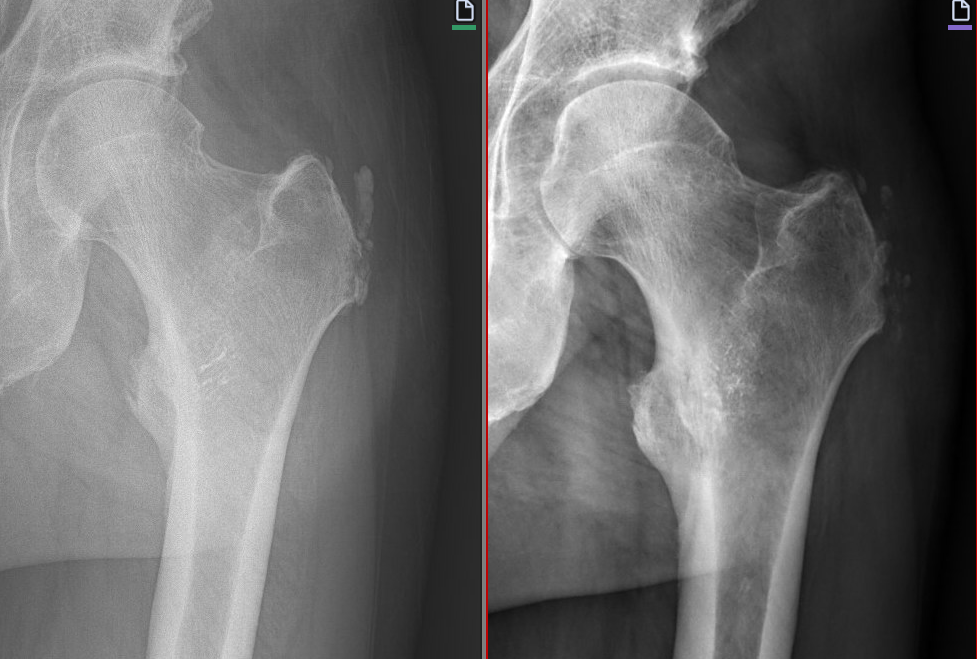
Tendinopathy encompasses a wide spectrum of tendon disease that includes both tendonitis (inflammation) and tendinosis (degeneration). Gluteal tendinopathy is a tendon disorder affecting tendons in the hips and buttocks area (also known as the gluteal region). These include the gluteus maximus, gluteus medius, and gluteus minimus, which run from the hipbone (pelvis) to the greater trochanter at the top of the thighbone (femur).
Physicians sometimes describe gluteal tendinopathy using other terminology, but it is important to know that these terms are not interchangeable. Some other terms that might encompass gluteal tendinopathy are:
- “Greater trochanteric pain syndrome,” or GTPS, as the tendons connect to the greater trochanter
- “Lateral hip pain,” as patients experience significant pain on the side of the hip
- “Trochanteric bursitis,” as up to 20% of patients with gluteal tendinopathy suffer from trochanteric bursitis
What are the common symptoms of gluteal tendinopathy?
Pain is often felt over the area near the top of the thighbone (the “greater trochanter”) and may extend down the side of the thigh.
The pain may worsen when:
- Climbing a staircase or a steep hill
- Getting out of bed from a lying or sitting position
- Lying on one side, especially the affected side
- Remaining seated for an extended period of time, especially when cross-legged
- Standing or balancing on one leg, often felt when putting on pants
Chronic hip pain caused by gluteal tendinopathy may feel severe. It can affect a patient’s physical activity, be detrimental to sleep, and negatively impact a patient’s ability to perform activities that many of us take for granted.
Who is at risk of gluteal tendinopathy?
Gluteal tendinopathy frequently impacts a wide variety of people and can occur from both tendon overuse or underuse. This is why gluteal tendinopathy is common in both athletes and non-athletes.
Younger people who run, ski, dance, or participate in physical activity that may lead to overuse or acute hip injuries, may experience gluteal tendinopathy. If a tendon injury is left untreated, continually exacerbated or not frequently utilized, the individual may develop chronic gluteal tendinopathy.
Women over 40 are also likely to experience gluteal tendinopathy, often due to the maturation process of aging and tendons becoming stiffer, decreasing their elasticity. Some evidence suggests that women who have completed menopause are more prone to hip pain and gluteal tendinopathy.
Gluteal Tendinopathy can also affect up to 1 in 3 people with low back pain.
What causes gluteal tendinopathy?
Gluteal tendinopathy can be a result of inflammation (tendinitis) after an injury or degeneration (tendinosis) when the tendon tissue degenerates or breaks down. The tendon is unable to transmit the compressive loads from the gluteal muscles to the greater trochanter, resulting in pain during movements that compress the tendon.
Potential causes of gluteal tendinopathy include:
- Overuse, or too much force placed on tendons during physical activities. Excessive compression of the hips, combined with high tensile loads within tendons, can result in an overuse injury and breakdown of the tendon structure.
- Compression of tendons after a fall or similar damage from an accident.
- Weight gain or obesity causing excess pressure on hip tendons.
- Underuse, or inactivity due to a sedentary lifestyle.
- Instability caused by wide hips or pelvis.
It typically takes longer to recover from chronic, degenerative gluteal tendinopathy or tendinosis than inflammatory gluteal tendinopathy or tendinitis. Rest typically does not help, but physical therapy exercises can ease symptoms.
How is gluteal tendinopathy diagnosed?
A physician may begin with a thorough examination of the hip, back, and pelvis to determine where the primary cause of the hip pain is located.
Using an MRI or ultrasound, a physician may look more closely at the tissue pathology to determine the presence of inflammation, degree of tissue breakdown, presence of calcium deposits, presence of tears, as well as rule out other conditions to confirm the diagnosis and determine a treatment plan.
How has gluteal tendinopathy traditionally been treated?
Historically, a few major treatment paths have been used for patients experiencing hip pain due to gluteal tendinopathy:
- Physical therapy exercises and corticosteroids. Basic physical therapy exercises can help strengthen gluteal muscles and relieve some of the pressure placed on the tendons that can lead to gluteal tendinopathy, while corticosteroid injections can help to reduce inflammation.
- Needle fenestration. This technique involves inserting a needle into the affected tendon, making micro punctures to encourage a natural inflammatory healing response.
- Prolotherapy or platelet-rich plasma injections. Prolotherapy involves multiple injections of an irritant solution, such as glucose, into the diseased tendon. Platelet-rich plasma injections include high concentrations of platelets derived from the patient’s blood to stimulate healing within the affected tendon.
- Bursectomy. Inflammation of the bursa (a fluid-filled sac that acts as a “cushion” between tissues in the tendon) can also lead to tendon pain in the hip and impact development of gluteal tendinopathy. By treating the inflammation in the bursa, a surgeon may be able to relieve some of the pain for the patient.
- Surgical repair. Often reserved for serious cases of chronic gluteal tendinopathy, surgical repair through open (or arthroscopic) surgery involves opening a patient’s hip to physically remove diseased tendon tissue.
Non-surgical treatments may be insufficient when the patient is diagnosed with tendinosis and often provide only short-term relief. Surgical treatments are associated with added anesthesia risk, recovery time, cost, and morbidity.
How does TenJet treat gluteal tendinopathy?
The patented TenJet device is specifically designed to treat tendinosis and calcification in tendons such as the gluteus medius, gluteus minimus, and gluteus maximus. It allows physicians to treat chronic gluteal tendinopathy in a safe, highly efficient, less invasive, and precise manner.
The procedure involves a small incision to guide the TenJet needle into the area of the degenerative tendon under ultrasound guidance. TenJet’s innovative design utilizes pressurized high-velocity jet of saline, as the cutting mechanism, to precisely remove calcifications and damaged tendinopathic tissue. In most cases, the procedure can be performed in an outpatient setting under local anesthesia.
What do recovery and rehab from gluteal tendinopathy look like?
Recovery from gluteal tendinopathy after an ultrasound-guided procedure using TenJet usually includes two weeks of rest and light activity, followed by physical therapy exercises.
Patients with adequate muscle strength may be allowed to walk without crutches immediately after the procedure. However, patients with muscle weakness, partial tear, or previous hip replacement, may be advised by their physician to consider a short-period of being non-weight-bearing and avoid walking or climbing. Patients may also be asked to sleep with a pillow between their legs to minimize pressure on the tendons.
The treating physician will guide their patient’s post-treatment recovery plan with specific physical therapy and home exercises customized to the patient to adequately strengthen the tendon as it heals after the procedure. Individual patient results may vary depending on a range of factors, but most patients experience significant relief within weeks following the procedure.
Anecdotal feedback suggests that patients experience faster recovery times and longer-lasting relief compared to more traditional treatments for gluteal tendinopathy.
Don’t let Hip Pain from Gluteal Tendinopathy Stand in the Way of Living Your Best Life
There’s no reason to live with the pain and discomfort caused by gluteal tendinopathy.
Patients diagnosed with tendinosis do not need to live with pain, go through a cycle of multiple non-surgical treatments, or fear the long recovery times associated with open or arthroscopic surgery. TenJet allows physicians to treat tendinosis using a minimally invasive technique with just a small incision, resulting in less downtime, fewer risks of complications, and less morbidity.
By choosing treatment with TenJet, patients with gluteal tendinopathy can find relief from chronic hip pain and return to living an active lifestyle.
Please click on the following links for additional resources
TenJet Patient Information
TenJet Physician Finder
TenJet Physician Information